Knowledge Center
September 14, 2023
What are Medical Devices to Prevent Pressure Injuries?
Patient positioning is vital in preventing tissue damage and pressure ulcers in the operating room. Proper patient positioning depends on the type and length of the procedure, anesthesia access to the patient, and the Pressure Relieving and Redistribution Devices being used.
Pressure-relieving and redistribution devices support and reduce the risk of developing peri-operative pressure injuries under bony prominences during surgeries.
In this article, you will learn:
- What are pressure ulcers (aka bed sores)?
- What is the difference between pressure relieving and pressure redistribution devices?
- How do pressure-relieving devices work?
- Commonly used pressure-relieving devices
- How do pressure redistribution devices work?
- Commonly used pressure redistribution devices
What are pressure ulcers (aka bed sores)?
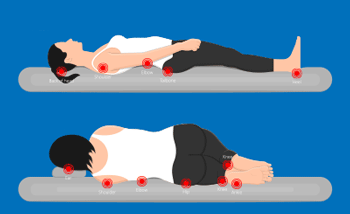
Pressure Ulcers are identified as localized damage to the skin or underlying soft tissue, usually occurring over a bony prominence due to pressure or pressure combined with shear or can be related to the use of medical or other devices.
Alternate names for pressure injuries are decubitus ulcer, bed sore, and pressure sore.
The intensity of the pressure, as well as the duration of the pressure, contribute to the injury.
Learn more about Pressure Ulcer Staging and Prevention Guide
What is the difference between pressure relieving and pressure redistribution devices?
Pressure relieving devices, like mattresses and gel positioners, improve the body contact area through envelopment/contouring and/or immersion. However, these devices do not provide active pressure reduction and possibly limit the redistribution the underlying surgical table pad offers. Pressure redistribution devices and surfaces use alternating air pressure to allow blood to flow (perfuse) back into the tissues. They can be used with redistribution devices like bean bags and gel pads.
How do pressure-relieving devices work?

Once patients are placed on these surfaces, they reactively or passively redistribute body weight. They work in response to the patient's weight and can fully compress under the patient. They may be powered or unpowered.
Immersive surfaces like these work at overall pressure reduction on certain patient surfaces, but even lower overall pressure over time can and does result in pressure injuries. This may not prevent a pressure injury on more lengthy procedures.
Commonly used pressure-relieving devices

Tabletop Pressure Management Pads:
They can come in sets or individual pads that attach to the surgical table or portable systems that go on multiple surfaces and environments.
Browse STERIS Pressure Management Systems
Gel cushions and positioners:
Used in supplement with tabletop pads for promotion of proper patient positioning. They can come in various shapes to support and protect different areas of the body like heels, elbows, sacral area, etc.
Browse STERIS Gel Positioners
Air-filled cushions:
These cushions are filled with air and can be adjusted to suit the individual's needs.
Foam cushions:
These cushions are made of foam, help to distribute pressure over a larger surface area, and can be disposable.
Browse STERIS Foam Positioners
Heel protectors:
These devices are worn on the heels to reduce pressure and prevent pressure injuries.
Browse STERIS Heel Protectors
Elbow protectors:
These devices are worn on the elbows to reduce pressure and prevent pressure injuries.
Browse STERIS Arm Protectors
How do pressure redistribution devices work?
These devices are active support surfaces, made of air cells that mechanically alternate the pressure beneath the body to reduce the duration of the pressure on the body by alternately inflating and deflating to change the contact area and, In other words, redistributing the pressure.
Redistribution devices are optimal for high-risk patients; can be used in all phases of perioperative care in pre-op, the operating room, and postop in PACU; operate with cyclical inflation and deflation; and require power.
Commonly used pressure redistribution devices
Alternating pressure mattresses:
These mattresses use air cells that alternate in inflation and deflation to help redistribute pressure.
Air-fluidized beds:
These beds use tiny silicone beads suspended in air, creating a fluid-like environment that helps redistribute pressure.
How do pressure relieving and distribution devices improve patient outcomes?
Reduce pain and discomfort.
Pressure relieving devices can help reduce pain and discomfort associated with pressure injuries, improving the patient's comfort.
Improve the quality of life.
By reducing the risk of pressure injuries, patients are more likely to maintain their independence and have a better quality of life.
Reduce healthcare costs.
Pressure injuries can lead to increased healthcare costs due to more extended hospital stays, additional treatments, and the need for specialized wound care. By preventing pressure injuries, pressure relieving devices can reduce healthcare costs.
Prevent complications.
Pressure injuries can lead to severe complications such as infections, sepsis, and death. Pressure-relieving devices can reduce the risk of these complications by preventing pressure injuries.
Reduce the risk of pressure injuries.
Pressure redistribution devices help to redistribute pressure over a larger surface area, reducing the pressure in any spot. This can help to prevent pressure injuries from developing in the first place.
Promote healing.
For patients with pressure injuries, pressure redistribution can help promote healing by reducing the amount of pressure on the affected area.
Reduce the need for additional treatments.
Pressure injuries can lead to the need for additional treatments, such as wound care or surgical interventions. By preventing pressure injuries, pressure redistribution devices can reduce the need for these other treatments.
Contributors

Lena Fogle BSN, RN, CNOR
Senior Director Global Clinical Solutions, STERIS Healthcare
![]()
Lena is a seasoned healthcare leader with extensive experience leading complex perioperative environments as well as new program development, continuous process improvement, clinical outcomes, operational excellence, and stakeholder experience.
References
- Guideline for pressure injury prevention. In: Guidelines for Perioperative Practice. Denver, CO: AORN, Inc; 2022.
- Shi C, Dumville JC, Cullum N et al. Beds, overlays and mattresses for preventing and treating pressure ulcers: an overview of Cochrane Reviews and network meta‐ analysis. Cochrane Database Syst Rev. 2021;8(8):CD013761.